
How can better data portability and access improve electronic health records in the UK? Danny Bluestone is the CEO of digital transformation agency and ODI Member Cyber-Duck
In April 2021, my mother went to hospital for a checkup and basic stent procedure, but ended up there for nearly a month – sent straight for an emergency triple bypass due to blocked arteries. Which, we were told, could have been avoided with earlier diagnosis and treatment. Yet a year earlier, she’d developed breathing difficulties on top of a history of high blood pressure and cholesterol (thus the stent procedure). So, what went wrong?
Prevention is always better than cure. I have asthma so am medically ‘proactive’ and use the NHS App to access my electronic health records (EHRs). EHRs aren’t new – countries like Israel and Estonia have already digitised their healthcare. There, the healthcare systems can notify patients about checkups, prescription dosages, and conditions they might be at risk of. Something that NHS EHRs do not do.
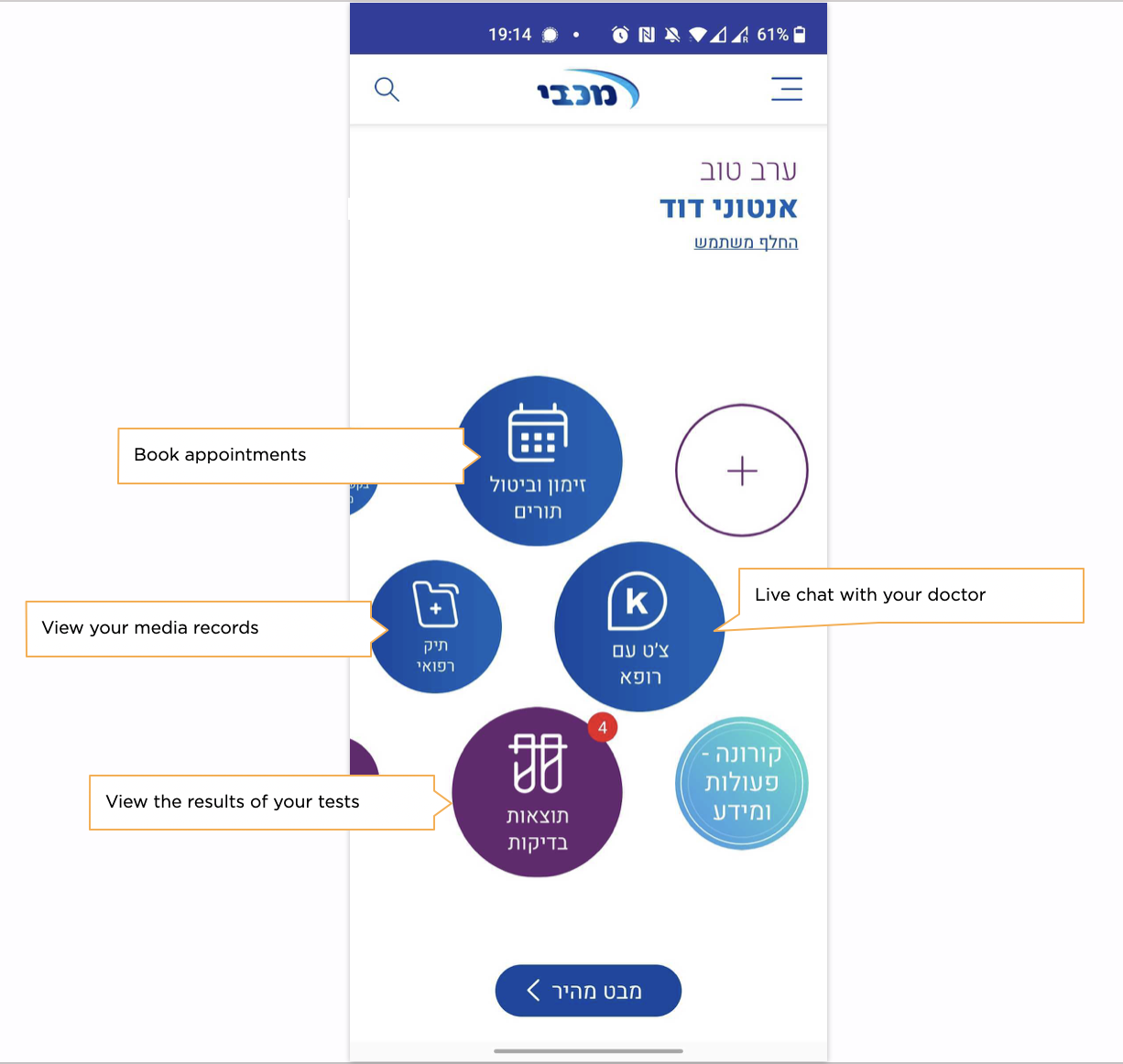
In my year of using it, the NHS app was passive: never pushing predictive information or preventative checkups my way. Even before my mother’s experience, since 2019, Cyber-Duck has been working on the question of how to explore EHRs to deliver better treatments and preventative healthcare services.
We found the fundamental challenges with EHRs are the ownership, portability, display, and access of data. But this can be overcome, as the examples of Israel and Estonia show, even though they are smaller countries. So why hasn’t this happened?
The current landscape
To understand this more fully, we must examine the landscape. The Labour government’s Health Record programme, spent £12.7bn on a digital patient record system that was later scrapped. And the Tories’ pledge for a paperless NHS by 2018, and 2020, never materialised.
There are multiple opposing political, cultural, structural, and environmental forces. Politically, we see NHS budgetary constraints and funding cuts. Environmentally, there is an ageing population with accompanying rising care costs, and, often, a lack of tech savviness.
Structural factors are significant. Most NHS hospitals still use localised, decentralised record-keeping. In 2018, 94% of NHS trusts still used handwritten notes for paper records. And IT systems are so dissimilar that they prevent interoperability, secure communication and data sharing.
Culturally, we are protective when it comes to data privacy. Research by Deloitte found that there was mistrust in what information is being gathered, who might access it, and how it might be used.
The NHS App
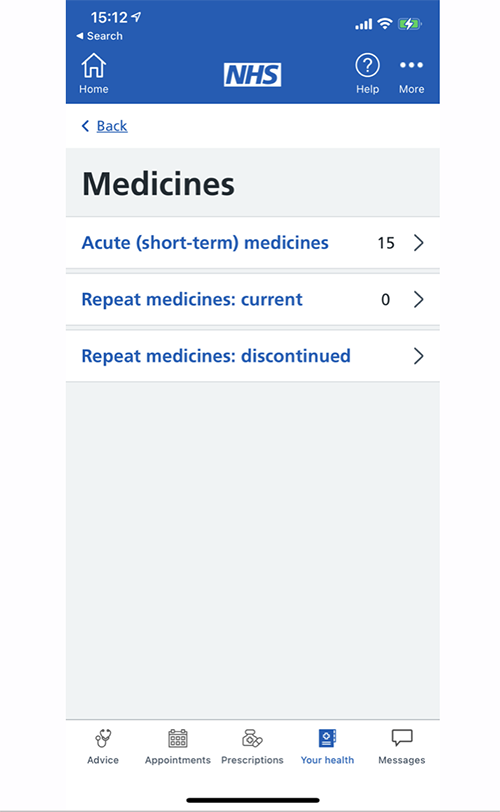
In 2019, NHS England launched the
, allowing patients to book appointments, view their records and order prescriptions. But the onus is on the patient to be proactive to their medical needs, with no automated reminders. Other features such as reviewing previous appointments or dependents’ records are unavailable.
There’s also ongoing user-experience problems. The app scrambles different purposes such as repeat prescriptions, a complex message interface, and various Covid-19 sections. Viewing records takes five or more taps with lots of scrolling, the only records are GP-prescribed medicines and Covid-19 vaccinations, none of it tailored or personalised.
Our solution
In 2019, Cyber-Duck ran a three-day hackathon, to design a workable EHR app using blockchain. We chose blockchain because it uses a distributed, immutable data format, not owned by any corporation or saved in a centralised database, thus tackling privacy and data ownership concerns. Blockchain uses a secure method called hashing to ensure all data (for example a medical note) can fit into 256 characters. Blockchain uses private keys to encrypt the data; public keys are then used to decrypt the data. In theory, this would allow a medical professional to view the EHR of any patient, which could be the difference between life and death in an emergency. Once a record is created, it then joins a ‘chain’ to include the previous hash of the prior record within the new hash, further increasing security. This decentralised blockchain approach can also tackle the big structural challenge of data portability and access. We identified the not-for-profit, open-source, health data interoperability effort, Standard Health Record Collaborative (SHRC), which gave each entity or asset – whether a condition, patient, practitioner, medicine or procedure – a semantical standard enabling it to be easily shared. At the time, the SHRC was sponsored by the US Department of Health and Human Services (HHS) and was recognised by NHS Digital.
Cyber-Duck’s EHR app
We developed our app with BigchainDB and used the JavaScript runtime Node.js to connect to the frontend application, as it’s designed to build scalable network applications, meaning it could realistically meet the needs of a country as large as the UK. Given most users would be using mobile devices, for the frontend, we chose a framework that included Web Workers and server-side rendering, improving performance and offering a smartphone-like experience. We needed something that was easy for all to use effectively, including the older community, and thus reduce NHS costs. So, we conducted actual audience research and common use cases to develop the user experience. Based on our research, the interface included:
- Medical events
- Appointments
- Messages/notifications
- Who accessed my data
- My conditions
- Relative (for example, dependent) management
- Person verification to further prevent misuse, and to increase trust for users.
The outcome

At Cyber-Duck, we have shown it is realistic to have an EHR app that meets our country’s size, structural setup, and data ownership requirements, while meeting users’ needs. Our proof of concept allowed hypothetical patients to access their medical information, sending alerts on prescription changes, upcoming checkups, and making patient information available only to verified hypothetical healthcare professionals.
Using automation, we leveraged one of the biggest benefits of digital technology: efficiency. It’s hard to quantify but imagine the savings and reduced burden on the system if it could have prevented my mother’s condition, instead of resulting in a costly emergency operation.
Thanks to emerging technology, we believe we can properly digitise our healthcare.
Fitbit can already keep records of your glucose levels
.
And, because of the pandemic, the NHS went from 20% remote primary care consultations to 90%, proving clinicians can work effectively remotely.
Our ultimate vision is better patient experiences, happier healthcare professionals, and a better economy. To get there, industry, government partners and healthcare providers must join together to make secure, accessible EHRs.